Foundation for Rural & Regional Renewal (FRRR)
Health care in rural areas is so often lacking and this scarcity of services, coupled with workforce shortages, means that many chronic health conditions are poorly managed and preventative health programs can be hard to find.
That’s why our Program Coordinator, Jeanice Henderson, was excited to travel to Kerang in northern Victoria last month to learn more about the progress of the innovative Rural Health Matters project.
Funded through an FRRR Enhancing Country Health Outcomes (ECHO) grant in 2020, Northern District Community Health (NDCH) is making good use of their $115,000 grant, funded by Beyond Medical Education. They have employed Emily Wood as Buloke, Loddon and Gannawarra (BLG) Project Coordinator, and are leveraging a truly inspirational health partnership spanning three Local Government Areas and multiple health services. This collaborative placed-based, systems approach is delivering a suite of local initiatives to help improve the current and emerging health needs for BLG Shire residents.
Plans for the original launch of the Rural Health Matters project were thwarted by COVID lockdowns. However, Mandy Hutchinson, CEO of NDCH said the delays meant the August event became a real celebration of what has been achieved so far and what is to come; a chance to share and applaud the amazing work and local partnerships that are starting to shift the dial on local health outcomes.
It was easy to see from the original grant application that a lot of the hard work had already been done. The BLG Local Health Community Services had researched and created the ambitious BLG Health Needs implementation plan, and made a solid start on various projects.
The FRRR ECHO grant is helping them to take this to the next level. Emily has been tasked with mapping the current health service provision across the three Shires and identifying the existing gaps and opportunities for further collaboration. She is also responsible for running a community awareness campaign for Heart Health risk factors; developing an allied health community of practice with a focus on chronic disease management and bringing people together for an annual chronic health forum; and working closely with new initiatives such as the Sustainable Rural Health Project.
Emily said that the ECHO grant for the Rural Health Matters (RHM) project has enabled a backbone for additional work to be developed, implemented, or supported and promoted across the BLG region.
“Alongside the identified KPI’s of the RHM project, there has been the opportunity to continue facilitation of an existing Chronic Disease Management: Community of Practice (COP) for allied health professionals and nurses which had previously had facilitation funding for 12 months through Murray PHN. This role enabled not only the continuation of the COP but also allowed me to act as a conduit between the systems level planning and the on the ground experience and feedback of the allied health staff – as was the case with the Murray PHN Sustainable Rural Health project.
“I have also been able to support the application for the Smoking Research Project, which has since been funded by the Department of Health. Currently the RHM project is also supporting the facilitation of a reference group for the Smoking Research Project and the development of an EOI for the position.
“Alongside this work, the RHM project has enabled me to participate in a range of BLG network meetings involving Community Health and Health Promotion – ensuring alignment of work and priorities where possible but also avoiding duplication. I’ve also been able to support and work closely with the Murray PHN Sustainable Rural Health Project, the AgriSafe Clinics at NDCH and both the MoveIT! Project and the Healthy Heart of Victoria project in Loddon.
“Lastly, it cannot be overlooked that the meetings of the BLG for the RHM project oversight also facilitated COVID coordination and support between local health services through sharing of learnings, experiences and challenges during meetings. The ongoing opportunity for the health services across the BLG region to discuss COVID at these meetings has not only strengthened relationships but created partnerships and pathways for support that will continue to benefit the BLG community.”
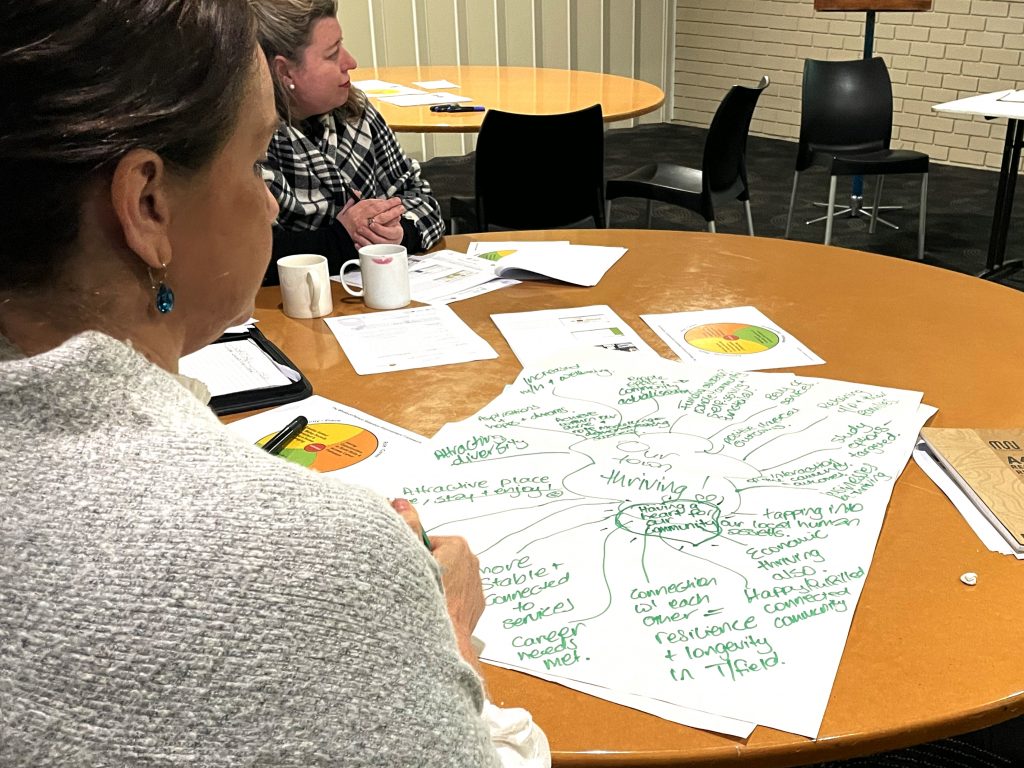
Jeanice said, “It was really heart-warming to see and feel the incredible level of genuine enthusiasm and commitment in the room on the day. The depth and breadth of collaboration between the groups represented at the event was amazing, but so too their willingness to seek greater collaboration with others. It was also inspirational and affirming to hear how the ECHO grant has triggered further investment.“
Nari Nari Country
On average, people in rural and remote Australia experience much higher rates of chronic disease, avoidable illness, and are far more likely to be hospitalised in circumstances where earlier access to the right care could have prevented it. Sadly, they also find it much harder to access allied health professional services: they are often thin on the ground or not there at all.
One of the main reasons for this is the difficulty in attracting and retaining rural health workers, leading to serious gaps and inequity in access to preventative and primary health care in rural and remote areas. While connection to community and place is increasingly being identified as an important factor for retention, there are few examples of how rural communities can foster or create these conditions in a systematic way.
But one organisation is trying to help resolve this. Services for Rural and Remote Allied Health (SARRAH) is a grassroots organisation advocating on behalf of rural and remote Australian communities to have access to allied health services. SARRAH is also the peak body representing rural and remote allied health professionals (AHPs) working in public, private and/or community settings.
They received a grant for just over $140,000 through FRRR’s Enhancing Country Health Outcomes (ECHO) program, funded by Beyond Medical Education, to address persistent rural health workforce shortages in small rural and remote towns in NSW and Victoria through a project leveraging Rural Health Workforce Coordinators (RHWC).
The project team is headed by Dr Cath Cosgrave, a leading research academic in the field of rural health workforce attraction and retention.
Generally, retention research has focused on the influence of organisational and role conditions, however how individuals feel and perceive their acceptance into a community is increasingly proving to significantly influence retention. Dr Cosgrave’s findings, along with other research, indicate that the decision of a health professional to take up, stay or leave a rural position involves personal, organisational and social considerations. People who relocate to a rural place for work and have persistent feelings of social alienation and loneliness will always leave, irrespective of whether the position is financially beneficial.
That’s the key insight that informed the creation of the Attract, Connect, Stay project, which is based on a successful model developed in Marathon, Canada. The translation of this model into the rural Australian context will benefit not just the communities involved in the project but develop tools and resources that can be applied more broadly.
The project involves a whole-of-community approach to supporting health professionals and their partners / families when moving into a new rural community to help them to feel settled, become socially connected, and experience a sense of belonging, all identified as essential conditions for retention.
Planning commenced with three New South Wales pilot local government areas in August 2021: Glen Innes, Gwydir Shire and Narrabri. These communities will be supported through a series of co-designed workshops to form a network of community, local government, businesses and health service representatives. These networks will go on to jointly develop, fund, recruit, appoint, manage and monitor the RHWC position and its’ success in attracting and retaining suitable health professionals to fill health service gaps in each community.
Learnings from the three NSW primary sites will be captured in prototype tools and resources, and further tested in two secondary sites in rural Victoria. The project will conclude with a launch of a purpose-built website where the refined tools and resources will be made available to the public. This will allow other communities to use the tools and resources to help design local approaches to address gaps in their own primary and preventative health workforces.
“We need to see more community-led and innovative projects like Attract, Connect, Stay to ensure rural and remote communities have access to health professionals to the same extent as their city-based counterparts.”
Cath Maloney, SARRAH CEO
Four rural health services in NSW and VIC awarded grants
The Foundation for Rural & Regional Renewal (FRRR) has awarded $368,768 in grants to four community health organisations in rural, regional and remote New South Wales and Victoria to enhance the primary and preventative health service offering in their communities.
Funded through the Enhancing Country Health Outcomes (ECHO) program, these grants will help to fill identified gaps in rural health workforce support and development, and the provision of accessible health care in areas where services are limited. Regions that are benefiting from these grants include the smaller communities surrounding the service centres of Nowra, Wagga Wagga, Armidale and Dubbo in NSW and Kerang, Wedderburn and Harrow in Victoria.
Natalie Egleton, CEO of FRRR, said that the ECHO program has provided insights into the various challenges facing health services in rural communities, and the continuing inequity of service access and provision.
“There’s a real need for flexible funding of community-based primary and preventative health services in rural communities, so it’s fantastic to be able to support local health initiatives through the ECHO program and help fill some of these gaps. Projects like Northern District Community Health’s place-based Rural Health Matters initiative will address health needs, health inequities and service provision gaps across several rural Victorian communities,” Ms Egleton said.
“There are also significant workforce shortages and limited access to upskilling and professional development opportunities for rural health services. We are pleased to be able to support the Cerebral Palsy Alliance in NSW and Harrow Bush Nursing Centre in Victoria. With these grants, these organisations can now undertake staff training and improve professional development opportunities throughout a number of rural communities.
“We are also pleased support an initiative lead by the Services for Australian Rural & Remote Allied Health, which will work with selected rural communities in both NSW and Victoria, helping communities to build their own capacity to attract and support a long-term rural workforce in their regions.
“This is the final round of the ECHO program, which was created thanks to a donation of just over $900,000 from Beyond Medical Education when they wound up. The program has highlighted the need for philanthropic support to help these local health services overcome health inequity in rural, regional and remote communities and we hope we can continue to help to fill these gaps,” Ms Egleton said.
Lynda Vamvoukis, former CEO of Beyond Medical Education, said that it is inspiring to see how Beyond Medical Education’s remaining funds have been used by groups to improve the local primary health care needs of the community.
“Building strong and sustainable relationships that support the health of these communities is critical. It has been rewarding to see this program support projects that foster this kind of long-term, health care provider collaboration,” said Ms Vamvoukis.
The four projects awarded grants this final round of the ECHO program are:
- Cerebral Palsy Alliance – Armidale, Dubbo, Nowra, Wagga Wagga, NSW – $80,000 – Improve access to, and delivery of services to people with a disability in rural communities by providing essential equipment, resources and training for rural therapists.
- Services for Australian Rural and Remote Allied Health – NSW and VIC – $140,179 – Address persistent rural workforce shortages in small rural and remote towns in NSW and Victoria through an Attract, Connect, Stay project leveraging Rural Health Workforce Coordinators.
- Harrow Bush Nursing Centre – Harrow, VIC – $33,589 – Increase organisational capacity and improve patient care by upskilling the existing rural workforce and upgrading the primary care vehicle to safely transport emergency equipment.
- Northern District Community Health – Kerang, Wedderburn, VIC – $115,000 – Improve the current and emerging health needs for Buloke, Loddon and Gannawarra Shire residents through the delivery of a collaborative placed-based systems approach
The Pain Revolution, in conjunction with the University of South Australia, set out to establish a community-led health initiative to promote best-practice pain management services in country NSW and Victoria, by raising awareness of pain neurobiology and the use of a bio-psycho-social pain model of education and care.
If that all sounds quite complicated, these facts are simpler to understand, though not very easy to digest:
- One in five Australians lives with chronic pain. In those over the age of 65, this increases to 1 in 3.
- According to The Pain Revolution, persistent pain is a bigger disability burden on rural Australia than cancer and diabetes combined.
- It is the most common reason for early departure from the workforce, and a known risk factor for severe depression and suicide.
What’s more, access to pain management services is poor in rural communities, and most attempts to address the problem include ‘travelling health teams’ and ‘country visits’ from city health specialists. With GPs reporting that they have insufficient knowledge, skill and self-efficacy to deliver best practice for persistent pain patients, The Pain Revolution stepped in to design a sustainable program of training, mentoring and resourcing with a focus on local capacity building.
Founded in 2017, The Pain Revolution is a cross sector collaboration led by Professor Lorimer Moseley from within the School of Health Science at the University of South Australia. It also draws on expertise from others working in the field, holding strong partnerships with the National Rural Health Alliance, Pain Australia, Australian Pain Society, the Australian Physiotherapy Association and the Australian College of Sports & Exercise Physicians. Their collective aim is to embed the capacity to deliver best practice pain education and care within rural and regional communities, and they are doing this through the Local Pain Collectives (LPC) program.

Pain science is an area with lots of interesting research and developments; new and effective approaches have been identified to prevent and manage persistent pain, placing emphasis on active approaches (movement and learning based) rather than passive ones (drugs, massage and surgery). These new self-management approaches can seem counter-intuitive amongst health professionals unless they have an understanding of contemporary pain science. International guidelines now universally recommend education as first-line treatment, but this is rarely delivered effectively as part of usual care.
The Pain Revolution determines where to target their efforts by assessing which rural and regional communities are flagged by the Australian Health Atlas as having excessive opioid prescriptions, back fusions and knee replacements. In response, the LPC program aims to upskill GPs and allied health professionals in best practise pain education and care within these communities, and establish a supported network amongst this difficult area of medical practice.
The Pain Revolution provided scholarships to twelve health professionals who live in regional communities across NSW/VIC. These individuals were trained to organise and deliver pain education events to the general public and other health professionals, and become clinical leaders and ‘champions for change’ within their community. Funding from the Enhancing Country Health Outcomes (ECHO) grant program enabled them to form a Local Pain Collective and deliver pain education in six regional areas of NSW: Wollongong, Nowra, Jindabyne, Cooma, Wagga Wagga and Albury/Wodonga.
Each Collective has delivered activities including pain education sessions, clinical support for knowledge to practice transfer, and a facilitated platform for peer-to-peer learning and resource sharing. A three-day workshop strengthened the network, bringing together the local pain educators, the reference group, content experts and facilitators, and monthly network meetings followed. The workshop also informed where skills could be developed, and this fed into the design and delivery of a monthly webinar series. Topics of direct relevance to the rural and regional context included understanding opioids, appraising evidence, facilitation skills, implementing behaviour change principles to pain care, and choosing words carefully when talking to pain patients.
In their application, Pain Revolution wrote that the project would deliver benefits on three levels. Of course it would benefit the rural and regional-based GPs and allied health professionals that participate. By improving pain education and care, it would also benefit the 1 in 5 rural Australians who suffer from persistent pain and the many more at risk of it because of a lack of up-to-date information and care.
The third level of benefit really speaks to the aims of the ECHO grant program:
“The extent to which persistent pain impacts entire communities – almost everyone is affected – means that this project will benefit entire communities by promoting informed self-management and resilience.”
FRRR is delighted to have been able to support this program, which is clearly making a difference to the lives of many rural people.
Grants of up to $150,000 available for Enhancing Country Health Outcomes
Bendigo, 5 May 2020: The Foundation for Rural and Regional Renewal (FRRR) is inviting not-for-profit organisations to apply for an Enhancing Country Health Outcomes (ECHO) grant to deliver initiatives that improve the health of people living in rural, regional and remote Victoria and New South Wales.
Rural communities face distinct challenges associated with distance and isolation, which place these regions at greater risk of poorer health management and outcomes than those living in metropolitan areas. In addition to these challenges, many parts of NSW and Victoria have been affected by drought, bushfires and now COVID-19, all of which have significant impacts on health care resources.
The ECHO grants program launched in 2018 thanks to a generous donation from Beyond Medical Education. The program offers targeted grants of between $50,000 and $150,000 for charitable initiatives delivered by not-for-profit organisations to strengthen, improve access to, and retain the quality of relevant and appropriate primary health care services in rural, regional and remote Victoria and NSW.
FRRR CEO, Natalie Egleton, says that basic health services, programs and equipment are vital to the sustainability of rural communities.
“Many of Victoria and New South Wales’ rural communities have limited access to appropriate primary health care. This has been compounded by the drought, bushfires, and now by the COVID-19 pandemic, and highlights the real need for communities to be able to attract resources and implement sustainable, best practice models that will see better health outcomes for local residents.
“Last year, we awarded $475,000 in grants through this program, and it’s great to see them making a real difference in the community. For example, Latrobe Community Health Service received a grant of $125,200 to implement the ‘Telkaya Project – Very Brief Advice For Behavioural Change’. Through this project, LCHS developed online training and support materials regarding lifestyle changes around smoking, nutrition, alcohol and physical activity. Staff are now able to integrate this intervention advice into their routine primary health care services.
“Mallacoota Community Health, Infrastructure and Resilience Fund, in Victoria, was another ECHO grant recipient, using $136,864 to help the local medical clinic get additional health services up and running. Patients can now access services including a general mental health program and Teen Clinic and a piloted nurse-led after-hours service, which has been particularly valuable given the impact of the fires,” said Ms Egleton.
Other types of rural and regional focussed projects that could be eligible include innovative primary health care training and leading-edge professional development to address an identified local need; measures to enhance the retention of primary health care services; or fostering local partnerships to develop better primary health care models. Full details and other examples are available in the program guidelines.
“The bushfires and COVID-19 have emphasised the real need for quality primary health services in rural and regional areas. Building strong and sustainable relationships that support the health of these communities is critical. It’s wonderful to be able to provide support for projects on the ground that foster this kind of long-term, health care provider collaboration,” said Ms Egleton.
Applications can be made via FRRR’s Grants Gateway, and close at 5pm AEST, 9 June 2020. Outcomes will be advised mid-August 2020.
Australian Institute of Health and Welfare (AIHW) statistics show that 50% of Australians have a common chronic health condition, such as diabetes, heart disease, a mental illness or cancer, and almost 25% have two or more of these conditions. Most of these chronic health conditions share preventable risk factors, such as smoking, excessive alcohol consumption, poor nutrition and being physically unfit (AIHW, 2018).
Statistics for Gippsland, in Victoria’s south east, indicate that residents have chronic disease risk factors well above the state averages (PHN, 2018). This is perhaps because the Aboriginal and Torres Strait Islander population in Gippsland is considerably higher than the rest of the state, with approximately 10% of Victoria’s Indigenous population living in this area (PHN, Gippsland, 2018). The Heart Research Institute (2018) states that Indigenous Australians are still around twice as likely to be affected by heart disease, twice as likely to have a heart attack, 10.5 times more likely to die from coronary heart disease and 1.2 times more likely to have high blood pressure than other Australians.
These prevalence rates prompted local health agencies to come together to identify new ways of getting key messages about health to those most at risk. The project was led by Latrobe Community Health Service (LCHS), a primary and community health service focused on providing patient-centred primary health care, especially for those with multiple health conditions and high support needs.
Other organisations involved include Gippsland Lake Health Service, Monash University Department of Rural Health and Ramahyuck Aboriginal District Corporation. Together, they have developed a face to face and online training package for nursing, allied health and Aboriginal health workers, in the effective and frequent delivery of health advice using the Very Brief Advice (VBA) format.
A VBA is a short and opportunistic health promotion message, delivered during routine clinical appointments and focused on encouraging patients to change habits. It involves pro-actively raising awareness of, and assessing a person’s willingness to engage in further discussion (advice) about unhealthy lifestyle issues. The Gippsland program is known as Health CHAT (Check, Hear, Advise, Talk). Key topics include smoking, nutrition, alcohol and physical activity.
A grant of $125,200 from FRRR’s Enhancing Country Health Outcomes (ECHO) program, funded by Beyond Medical Education, enabled LCHS to engage a part-time Project Manager to lead the project. The grant also covered costs of filming and development of the online training education modules.
A steering committee was formed to oversee the development of the training content. An Aboriginal liaison support worker from LCHS provided feedback on the training modules to ensure the materials are culturally appropriate and relevant to the local Aboriginal community members.
Four instructional videos were developed, which included interviews with healthcare workers as well as people who use or volunteer at each of the services. A training package accompanies the instructional videos to ensure allied health and nursing staff have the knowledge, confidence and skills to deliver the Healthy CHAT program in their everyday practice.
The online modules were piloted with multiple stakeholders and key staff, before being rolled out to around 50 health care workers at two LCHS community health services and one LCHS Aboriginal health service in the Gippsland area. The online learning modules and other useful resources are now available on the Healthy CHAT website.
The grant also provided funding for formal evaluation and a structured approach to assessing the changes in knowledge, confidence and attitudes about delivering Healthy CHAT, which was completed in December 2019. It is hoped that this pilot project will provide a proven way forward for other rural, regional and remote clinical settings, especially in reaching groups with lower health literacy and/or who are socially and economically disadvantaged.
$475,000 in grants to help local organisations address health care gaps
Bendigo, 27 September 2018: The Foundation for Rural and Regional Renewal (FRRR) today announced that four organisations will share in over $475,000 to implement vital health services in rural and regional communities in NSW and Victoria.
The Enhancing Country Health Outcomes (ECHO) program was established to provide grants for charitable initiatives that strengthen, improve accessibility and retain quality primary health care services in local communities. Distance and isolation place rural and regional communities at greater risk of poorer health outcomes and management. Basic health services, programs and equipment are vital to the sustainability of small communities. The funding for this program comes via Beyond Medical Education, which closed and transferred their funds to FRRR.
Demand for this new program was strong, with FRRR receiving 27 applications requesting nearly $3 million toward projects valued at $5.8 million. Acting CEO Sarah Matthee says that this shows the high level of need for improved access to health services across rural, regional and remote Australia.
“Through ECHO, we are supporting small communities to improve accessibility and implement sustainable, contextually appropriate responses to help the local residents live well in their communities. The four grants will support these organisations to up-skill the rural health workforce and implement innovative responses to provide a better service for clients,” said Ms Matthee.
Lynda Vamvoukis, a former CEO of Beyond Medical Education, said she was impressed by the applications received and that she is confident the four successful organisations will address the day-to-day health care needs in these small communities.
“No matter where you live, quality primary health services are vital in a community. This program provides support to ‘on the ground’, multidisciplinary and integrated projects that respond to specific primary health care issues within a local community,” said Ms Vamvoukis.
The following organisations will receive large-scale grants to implement locally led solutions:
- NSW Outback Division of General Practice Ltd – $111,000 to re-establish an Occupational Therapist (OT) based in Bourke, NSW. The OT will be part of a multidisciplinary team, supporting the therapy services provided from clinical hubs in Bourke and the surrounding towns of Louth, Wanaaring, Enngonia, and Brewarrina. The OT service will provide one-to-one early intervention and support for children with delayed development, to ‘at risk’ groups such as adults with mobility issues, and enable people to access specialist and ongoing support services where available and appropriate.
- Mallacoota Community Health, Infrastructure and Resilience Fund Inc. (CHIRF), in Victoria – $136,864 to support the development and implementation of additional health services through the local medical clinic. Services will include a general mental health program, Teen Clinic, piloting a nurse-led after-hours service, and maintaining the Dr Search workforce recruitment program. Funds will also support a Project Manager to develop these additional services.
- Latrobe Community Health Service (LCHS), in Victoria – $125,200 to implement the ‘Telkaya Project – Very Brief Advice for behavioural change’, focusing on lifestyle changes around smoking, nutrition, alcohol and physical activity. LCHS will work with Gippsland Lake Health Service, Monash University Department of Rural Health and Ramahyuck Aboriginal District Corporation to develop an online training package and support materials to build the capability of LCHS and staff to integrate brief invention advice into routine primary health care services.
- University of South Australia will receive $102,500 for Stage 2 of the Local Pain Educator (LPE) program. Conducted by Pain Revolution, this is a community-based health education initiative focuses on building the skills and capacity of local health professionals to support people living with chronic pain, reducing the reliance on strong opioids. With this grant, Local Pain Networks will be established across five regional areas surrounding Cooma, Nowra and Wagga Wagga in NSW, Albury-Wodonga NSW / Vic border and Warracknabeal, Vic.
New program offers grants up to $150,000 in rural NSW and VIC to improve health services
Bendigo, 31 May 2018: It’s no secret that distance and isolation place rural and regional communities at greater risk of poorer health outcomes and management. To provide much-needed support, the Foundation for Rural and Regional Renewal (FRRR) has launched a new funding program that will help to improve health outcomes for people living in rural, regional and remote New South Wales and Victoria.
The Enhancing Country Health Outcomes (ECHO) program will provide grants for charitable initiatives that strengthen, improve accessibility and retain quality primary health care services in local communities.
The funding for this program comes via Beyond Medical Education, which closed down due to changes in government policy and transferred their funds to FRRR. Thanks to this generous donation, grants of up to $150,000 are available for projects to be delivered over two-years from October 2018. Approximately $ 825,000 is available over two rounds.
FRRR CEO, Natalie Egleton says that priority will be given to locally driven initiatives that support primary health care.
“Basic health services, programs and equipment are vital to the sustainability of small communities. Through ECHO, we can support local communities to attract resources and implement best practice sustainable models to help local residents to live and thrive in their communities.
“FRRR has previously supported a number of projects that achieved better health outcomes for community members. For example, we funded the Australian College of Optometry to purchase a slit lamp to enhance the level of eye care in Ouyen, Victoria. Patients can now receive early intervention and be treated locally rather than travelling 100 km for specialist appointments. This program will mean that there can be more of these kinds of local initiatives,” said Ms Egleton.
Other projects that could be eligible include primary health care training and leading-edge professional development in a rural and remote context; measures to enhance the retention of primary healthcare services in rural and remote locations; or fostering local partnerships to develop better primary health care models in their community. Full details and other examples are available in the program guidelines.
Lynda Vamvoukis, a former CEO of Beyond Medical Education, said that in gifting the remaining funds to FRRR, the Board wanted to ensure funds were available to community groups that are focused on addressing local primary health care needs.
“Quality primary health services and building long term, sustainable relationships are critical, especially in rural and regional areas. This program provides support on the ground for collaborative, multidisciplinary and integrated projects that respond to specific primary health care issues within a local community,” said Ms Vamvoukis.
Applications for the ECHO program close on 9 July 2018.